Abstract
Background: Acute graft-versus-host-disease (aGVHD) is one of the main complications after allogeneic hematopoietic stem cell transplantation (allo-HSCT), occurring in about half of patients. Patients with grade II-IV aGVHD require treatment with systemic corticosteroids. However, 30% of them show steroid resistance, leading to poor prognosis. Thus, pretreatment prediction of steroid refractoriness allows for early secondary treatment introduction, which may improve aGVHD outcomes. The possible association between elevated peripheral blood (PB) eosinophil counts and the development of aGVHD has been previously reported. In contrast, several studies showed an association with better outcomes after allo-HSCT. These reports imply that PB eosinophil counts may predict prognosis in patients with aGVHD. In this study, we investigated the predictive role of pretreatment PB eosinophil counts in patients with aGVHD treated with systemic corticosteroid therapy.
Methods: Retrospective case analysis was performed on 121 patients with hematological malignancies who underwent allo-HSCT between October 2010 and January 2017 in our institutes and developed any grade of aGVHD. We excluded patients who did not require systemic corticosteroid therapy (n=53), and who developed aGVHD after premature discontinuation of calcineurin inhibitors (n=5) because of relapse or calcineurin toxicities. Finally, a total of 63 patients were enrolled. PB smears obtained within 2 days before the start of systemic corticosteroid therapy were microscopically examined. The cut-off value of eosinophil counts for predicting survival was determined using receiver operating characteristic (ROC) curve analysis. The primary endpoint was 1-year overall survival (OS), measured from the start of systemic corticosteroid therapy to death due to any cause or the last follow-up. The secondary endpoints were 1-year progression-free survival (PFS), 1-year cumulative incidence (CI) of non-relapse mortality (NRM), and CI of relapse. OS and PFS were compared using the log-rank test and CIs of NRM and relapse were compared using Gray's test. Predictors of OS were evaluated using univariate and multivariate analysis using Cox's proportional hazards model.
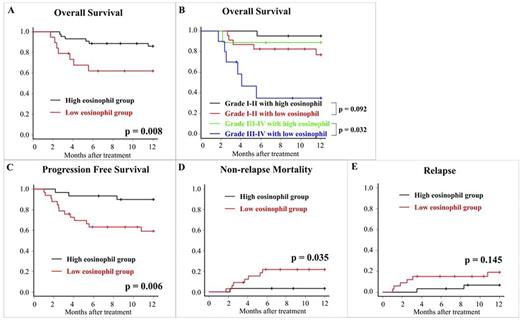
Results: The median age was 48 years (range: 40-59 years), and 31 patients (60.8%) were male. Primary diagnoses were acute myeloid leukemia (n=21), acute lymphoblastic leukemia (n=18), myelodysplastic syndrome (n=9), malignant lymphoma (n=13), multiple myeloma (n=1), and chronic myelomonocytic leukemia (n=1). They received bone marrow (n=38), peripheral blood stem cells (n=5), and cord blood (n=20). The median PB eosinophil count was 96/mm3 (range: 0-2903/mm3). ROC analysis revealed the cut-off value for predicting 1-year OS as 133/mm3 (area under the curve: 0.783; 95% confidence interval, 0.662-0.904). Thus, we defined patients with eosinophil counts ≥133/mm3 as the "high eosinophil group" (n=30) and the others as the "low eosinophil group" (n=33). There was no difference in clinical characteristics between the two groups, with the exception of days from transplantation to systemic corticosteroid therapy (29 days in the low eosinophil group vs. 43 days in the high eosinophil group, p<0.001). Regarding the primary endpoint, the 1-year OS rates were 65.2% and 93.3% in the low and high eosinophil groups, respectively (p=0.008) (Figure A). In the univariate analysis, the hazard ratio (HR) for 1-year OS of the low eosinophil group was 6.0 (95% confidence interval: 1.3-27.2, p=0.020). In the multivariate analysis adjusted for eosinophil counts (low vs. high), recipient age (≥50 vs. <50 years), aGVHD grade (III-IV vs. I-II), and stem cell source, the low eosinophil group showed independent poor prognosis for 1-year OS (HR, 6.0; 95% confidence interval, 1.3-28.4; p=0.023). Especially in patients with grade III-IV aGVHD, the low eosinophil group showed substantially inferior 1-year OS rates than those in the high eosinophil group (35.0% vs. 88.9%, p=0.032) (Figure B). Regarding secondary endpoints, 1-year PFS rates were 59.2% and 89.9% (p=0.006), 1-year CI rates of NRM were 21.7% and 3.33% (p=0.035), and 1-year CI rates of relapse were 19.1% and 6.8% (p=0.145) in the low and high eosinophil groups, respectively (Figures C-E).
Conclusion: Low PB eosinophil counts before systemic corticosteroid therapy is associated with inferior 1-year OS after aGVHD due to elevated NRM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal